Weight gain is one of the most common and frustrating side effects people worry about when starting antidepressant medication.
For many individuals already struggling with depression or anxiety, changes in body weight can negatively impact self-esteem, motivation, and overall mental well-being.
This concern often leads people to delay treatment, stop taking prescribed medication, or avoid antidepressants altogether even when they could significantly improve quality of life.
The good news is that not all antidepressants cause weight gain. Some medications are considered weight-neutral, while others may even be associated with mild weight loss in certain individuals.
Understanding how different antidepressants affect appetite, metabolism, and energy levels can help patients and healthcare providers make better, more personalized treatment decisions.
In this article, we’ll explore antidepressants that don’t cause weight gain, explain why some medications affect weight more than others, and discuss evidence-backed options that support both mental health and physical well-being.
With the right information and medical guidance, it’s possible to manage depression effectively without sacrificing weight goals.
How Antidepressants Affect Body Weight
Antidepressants can influence body weight in several complex ways, and the effects vary widely from person to person. One of the primary reasons weight changes occur is the way these medications interact with neurotransmitters such as serotonin, dopamine, and norepinephrine—chemicals that regulate mood, appetite, hunger signals, and energy balance. When these systems are altered, appetite and food preferences may change, sometimes leading to increased calorie intake.
Some antidepressants stimulate appetite by enhancing cravings for carbohydrates and sugary foods, while others may slow metabolism or reduce energy levels, making physical activity more difficult. Sedation and fatigue are common side effects of certain medications, which can indirectly contribute to weight gain by lowering daily movement and exercise.
It’s also important to note that improvement in depression itself can affect weight. People experiencing severe depression often have reduced appetite and unintended weight loss. As symptoms improve with treatment, appetite may return to normal, which can be mistaken for medication-induced weight gain.
Duration of treatment plays a role as well. Short-term use of some antidepressants may not significantly affect weight, while long-term use can lead to gradual changes over months or years. Additionally, individual factors such as genetics, age, hormonal balance, lifestyle habits, and underlying medical conditions all influence how the body responds to antidepressant therapy.
Understanding these mechanisms helps explain why some antidepressants are more weight-neutral than others and highlights the importance of personalized treatment choices.
Factors That Determine Whether You Gain Weight on Antidepressants
Weight changes on antidepressants are not caused by medication alone. Several individual and treatment-related factors play a significant role in determining whether someone gains, loses, or maintains weight while taking these drugs. Understanding these factors can help set realistic expectations and guide better decision-making.
Genetics and metabolism are major influences. Some people are naturally more sensitive to appetite changes or metabolic shifts caused by antidepressants, while others experience little to no impact. Age and sex also matter, as metabolic rate tends to slow with age, and hormonal differences can affect fat storage and hunger signals.
Dosage and duration of treatment are equally important. Higher doses and long-term use are more commonly associated with gradual weight gain, especially if dietary habits and activity levels are not adjusted. Early weight changes often predict long-term trends, which is why monitoring during the first few months is crucial.
Lifestyle factors such as diet quality, physical activity, sleep, and stress levels can either worsen or offset medication-related weight effects. Poor sleep and chronic stress, for example, increase cortisol levels, which can promote fat storage regardless of medication type.
Underlying health conditions also play a role. Disorders like hypothyroidism, polycystic ovary syndrome (PCOS), insulin resistance, and anxiety disorders can amplify weight gain risks.
Because of these variables, two people taking the same antidepressant may have completely different weight outcomes, reinforcing the need for individualized treatment and ongoing medical supervision.
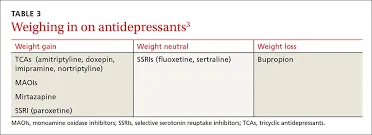
Antidepressant Classes and Their Typical Weight Effects
Different classes of antidepressants affect body weight in different ways, largely due to how they act on brain chemistry and bodily systems. Understanding these classes helps explain why some medications are more likely to be weight-neutral than others.
SSRIs (Selective Serotonin Reuptake Inhibitors) are among the most commonly prescribed antidepressants. They work by increasing serotonin levels, which can initially reduce appetite in some people. However, long-term SSRI use may lead to weight gain for certain individuals, particularly with medications that strongly influence appetite and carbohydrate cravings. Not all SSRIs behave the same—some are more weight-neutral than others.
SNRIs (Serotonin–Norepinephrine Reuptake Inhibitors) affect both serotonin and norepinephrine. This dual action can increase energy expenditure and reduce fatigue, making SNRIs generally more weight-neutral compared to many SSRIs. Some people even experience mild appetite suppression, especially during the early stages of treatment.
Atypical antidepressants have unique mechanisms of action and are often preferred for patients concerned about weight. These medications may target dopamine and norepinephrine rather than serotonin alone, which can help regulate motivation, energy levels, and appetite more effectively.
In contrast, older antidepressants, such as tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs), are more strongly associated with weight gain. They often cause sedation, increased appetite, and metabolic changes, which is why they are typically reserved for cases where newer medications are ineffective.
Overall, newer antidepressant classes tend to offer better weight profiles, but individual responses still vary. Choosing the right class is a critical step in minimizing unwanted weight changes while treating depression effectively.
Antidepressants Least Likely to Cause Weight Gain
For individuals concerned about weight changes, several antidepressants are considered weight-neutral or weight-friendly based on clinical evidence and patient reports. These medications are often preferred when weight management is an important part of overall health.
Bupropion (Wellbutrin) is widely recognized as the antidepressant least likely to cause weight gain. It works by increasing dopamine and norepinephrine rather than serotonin, which can help reduce appetite and increase energy levels. Many patients experience mild weight loss, making it a popular option for those with depression and weight concerns. However, it may not be suitable for individuals with a history of seizures or eating disorders.
Fluoxetine (Prozac) is another antidepressant often associated with minimal weight gain. In the short term, it may suppress appetite and lead to slight weight loss. Over long-term use, weight changes are generally modest compared to other SSRIs.
Sertraline (Zoloft) tends to have a more moderate weight profile. While some people experience weight gain over time, many maintain stable weight, especially when lifestyle habits are well managed.
SNRIs such as Venlafaxine (Effexor) and Duloxetine (Cymbalta) are generally considered weight-neutral. Their energizing effects may help counter fatigue and support physical activity, reducing the likelihood of weight gain.
It’s important to remember that no antidepressant is completely weight-risk-free. Individual response varies, and the best option depends on mental health needs, medical history, and long-term treatment goals.
Antidepressants More Likely to Cause Weight Gain
While many newer antidepressants have more favorable weight profiles, some medications are consistently associated with weight gain, especially during long-term use. Understanding which antidepressants carry higher risk can help patients and clinicians make informed treatment decisions.
Mirtazapine (Remeron) is one of the antidepressants most strongly linked to weight gain. It increases appetite and cravings, particularly for carbohydrates, and has a sedating effect that can reduce physical activity. Although it can be highly effective for depression, anxiety, and sleep disturbances, weight gain is a common trade-off.
Paroxetine (Paxil), an SSRI, is also known for causing more weight gain compared to other medications in its class. It can increase appetite and may slow metabolism over time, making weight management more challenging for some users.
Tricyclic antidepressants (TCAs) such as amitriptyline and nortriptyline are older medications that frequently lead to weight gain. They often cause sedation, dry mouth, and increased hunger, which together promote higher calorie intake and reduced activity.
Monoamine oxidase inhibitors (MAOIs) can also contribute to weight gain, partly due to dietary restrictions that encourage higher-calorie “safe” foods and changes in metabolism.
Despite their weight-related side effects, these medications may still be appropriate in certain cases, particularly when other treatments have failed. In such situations, close monitoring, dietary adjustments, and lifestyle strategies become essential to minimize weight-related impacts while maintaining mental health stability.
What Scientific Studies Say About Antidepressants and Weight
Scientific research shows that the relationship between antidepressants and weight change is complex and often misunderstood. Large-scale studies and long-term clinical trials suggest that weight effects vary not only by medication but also by duration of use and individual response. Short-term studies, typically lasting a few weeks to months, often show little to no weight gain for many antidepressants. However, longer studies reveal that gradual weight changes can occur over time.
Research consistently identifies bupropion as the antidepressant most likely to be associated with weight loss or weight neutrality. In contrast, medications such as mirtazapine, paroxetine, and tricyclic antidepressants show a higher average weight gain, especially after six months to a year of continuous use. SSRIs like fluoxetine and sertraline tend to fall somewhere in the middle, with modest long-term changes for many patients.
Another important finding is that early weight changes often predict long-term outcomes. Patients who gain weight within the first three to six months are more likely to continue gaining weight, while those who remain stable early on often maintain their weight long term.
Despite these insights, studies also highlight significant limitations. Many trials rely on self-reported weight data, have short follow-up periods, or fail to account for lifestyle factors such as diet and physical activity. This variability explains why personal experiences can differ widely from study averages, reinforcing the importance of individualized monitoring and treatment adjustments.
Weight Gain vs Mental Health: Risk–Benefit Analysis
When considering antidepressants, it’s important to weigh the mental health benefits against potential physical side effects, including weight gain. Depression is a serious condition that can significantly impact quality of life, relationships, and overall health. While weight changes are concerning for many patients, untreated or inadequately treated depression can have far-reaching consequences, including worsening mood, anxiety, fatigue, and even increased risk of chronic health problems.
For some medications, a modest weight gain may be an acceptable trade-off if the antidepressant effectively relieves depressive symptoms, improves energy, and restores daily functioning. Clinicians often recommend focusing on overall well-being rather than just the scale, particularly when a medication has proven efficacy for a patient’s specific symptoms.
Conversely, for patients who are particularly sensitive to weight changes, weight-neutral antidepressants like bupropion, fluoxetine, or certain SNRIs may offer a better balance between mental and physical health. In some cases, combining medication with lifestyle strategies—such as a balanced diet, regular physical activity, and sleep management—can further reduce the risk of weight gain while maximizing therapeutic benefits.
Ultimately, the key is personalized treatment. Decisions about antidepressant selection should consider medical history, mental health needs, lifestyle factors, and patient priorities. Working closely with a healthcare provider allows patients to achieve symptom relief without compromising long-term physical health.
How to Prevent or Minimize Weight Gain on Antidepressants
Even when taking antidepressants that have a higher likelihood of weight gain, there are practical strategies to prevent or minimize unwanted changes. Combining medical guidance with lifestyle adjustments can make a significant difference in maintaining healthy weight while managing depression effectively.
1. Nutrition Strategies: Monitoring diet is one of the most effective ways to control weight. Focus on high-protein, high-fiber foods that promote satiety and reduce overeating. Limiting added sugars, refined carbohydrates, and processed snacks can help counteract medication-related appetite increases. Planning meals and snacks in advance, as well as keeping a food journal, can provide insight into eating patterns influenced by medication.
2. Physical Activity: Regular exercise not only helps maintain a healthy weight but also supports mental health. Cardiovascular activities like walking, jogging, or cycling, combined with strength training, can boost metabolism and offset potential weight gain. Even light daily activity, such as taking stairs or short walks, can help maintain energy balance over time.
3. Sleep and Stress Management: Poor sleep and chronic stress elevate cortisol levels, which can promote fat storage and cravings. Prioritizing sleep hygiene, relaxation techniques, and mindfulness practices can reduce these effects and improve overall well-being.
4. Medication Management: Always discuss weight concerns with your doctor. Adjusting dosage, switching to a weight-neutral antidepressant, or combining medications strategically can help reduce weight-related side effects without compromising treatment effectiveness.
By integrating these approaches, patients can maintain both mental and physical health, ensuring that antidepressant therapy supports overall well-being rather than creating new challenges.
Choosing the Right Antidepressant With Your Doctor
Selecting an antidepressant is not a one-size-fits-all process, and weight considerations are only one part of a larger treatment plan. The right medication should balance effectiveness for mental health symptoms with minimal side effects, including weight gain, sedation, or appetite changes. Collaboration with a healthcare provider is essential to achieve this balance.
When discussing options, it’s important to consider your medical history. Conditions like diabetes, thyroid disorders, or metabolic syndrome can influence how your body responds to antidepressants and how susceptible you are to weight changes. Your doctor will also take into account past experiences with medications, including what worked, what didn’t, and any side effects previously encountered.
Patient priorities play a crucial role as well. Some individuals may tolerate minor weight gain if it means significant improvement in mood, energy, and functionality, while others may prioritize weight neutrality due to personal health goals or self-esteem concerns. Open communication about these preferences helps the provider tailor the medication choice accordingly.
Other considerations include co-existing mental health conditions, such as anxiety, insomnia, or chronic pain, which may influence the choice of antidepressant. For instance, mirtazapine may be selected for patients struggling with insomnia but comes with higher risk of weight gain, whereas bupropion may be ideal for those concerned about weight or low energy.
Ultimately, choosing the right antidepressant involves a risk–benefit analysis, combining clinical evidence with individualized care. Regular follow-ups allow adjustments to dosage, switching medications if necessary, and ongoing monitoring of both mental and physical health outcomes.
Myths and Misconceptions About Antidepressants and Weight
Many people avoid or discontinue antidepressants due to concerns about weight gain, but several common myths often exaggerate the risk or misrepresent reality. Understanding the facts can help patients make informed decisions and reduce unnecessary anxiety about treatment.
Myth 1: All antidepressants cause weight gain.
Not all antidepressants affect weight in the same way. While some medications, like mirtazapine or paroxetine, are more likely to cause weight gain, others such as bupropion, fluoxetine, and certain SNRIs are considered weight-neutral or even slightly weight-reducing in some individuals.
Myth 2: Weight gain is unavoidable.
Weight changes are influenced by multiple factors, including diet, activity level, metabolism, and genetics. With proper lifestyle strategies and regular monitoring, many patients can maintain stable weight while on antidepressants.
Myth 3: Stopping antidepressants is safer than gaining weight.
Discontinuing antidepressants without medical guidance can lead to worsening depression, withdrawal symptoms, and relapse. In most cases, managing weight through nutrition, exercise, or switching to a weight-neutral medication is safer than stopping treatment abruptly.
Myth 4: Weight gain indicates the medication isn’t working.
Weight changes do not correlate with antidepressant effectiveness. A medication may be relieving depressive symptoms effectively even if mild weight gain occurs, highlighting the importance of prioritizing mental health outcomes alongside physical health.
Dispelling these myths encourages patients to approach treatment with realistic expectations, empowering them to manage both mental health and weight effectively under professional supervision.
FAQs About Antidepressants and Weight
Patients often have specific questions about how antidepressants affect weight, and addressing these can help clarify concerns and guide safe, informed treatment decisions.
1. Which antidepressant causes the least weight gain?
Bupropion (Wellbutrin) is widely considered the least likely to cause weight gain and may even contribute to mild weight loss. Fluoxetine (Prozac) and certain SNRIs like venlafaxine and duloxetine are generally weight-neutral for most patients.
2. Can antidepressants cause weight loss?
Yes. Bupropion is the most notable antidepressant associated with weight loss, likely due to its effects on dopamine and norepinephrine, which can reduce appetite and increase energy. Some patients may also experience mild appetite suppression with fluoxetine.
3. Is weight gain from antidepressants permanent?
Not necessarily. Weight gain can often be managed or reversed with lifestyle interventions such as balanced nutrition, regular exercise, and adequate sleep. Switching to a weight-neutral antidepressant may also help.
4. How long does it take to notice weight changes?
Weight changes typically appear within a few weeks to several months of treatment. Early monitoring is important, as initial trends often predict long-term outcomes.
5. Can switching antidepressants help stop weight gain?
Yes. If a patient experiences significant weight gain on a particular medication, doctors may recommend switching to a weight-neutral option while monitoring mental health symptoms to ensure effectiveness.
Answering these common questions reassures patients that weight management is possible while receiving effective depression treatment, emphasizing the importance of personalized care and ongoing medical supervision.

I’m the Joke Master behind JokeDrops.com. I live to make people laugh with clever puns, funny lines, and daily humor drops. Spreading smiles is my favorite job — one joke at a time!